When Dr. Jan Andrysek was a master’s student at Holland Bloorview Hospital in 1998, he was already working alongside rehabilitation engineers and clinicians to develop solutions to help kids walk.
“There were a lot of gaps in terms of prosthetic technology that, particularly kids, which make a bit of a niche group”, says Jan, “My project at the time was to design a pediatric prosthetic knee joint. At the time prosthetics were not durable enough for kids, and they didn’t provide the function that was needed. We didn’t get to a solution at the end of my masters, but I did get an understanding of what worked and what didn’t work.”
Fast forward 21 years, Jan’s research project has already developed a niche within the prosthetic rehabilitation community. While running his research lab at the Holland Bloorview Children’s Rehabilitation Hospital, Jan patented this knee joint technology and brought it to market via LegWorks, a Canadian company co-founded by Jan in 2014. Under the brand name of All-Terrain Knee, more than 2,000 units were sold across 40 countries over the past several years. “What distinguishes our device from others on the market is its durability, cost effectiveness, and functionality. MaRS Innovation, Holland Bloorview Hospital, and Grand Challenges Canada have all been investors in the past.”
In Canada, the cost of an entire prosthetic leg would range from $5,000 to $10,000 for low end, and up to $100,000 for devices with heavy digital components. For the knee component, it would cost around $5,000 alone. While clients in developed countries are generally reimbursed via insurance for these prosthetic devices, the accessibility of these devices in developing countries is stymied by the cost.
“80% of the world do not have access to prosthetic technology,” says Jan, “We are in the business of helping people, and if existing prosthetic devices are not reaching a wide audience, we are doing something terribly wrong.” In Tazania, Kenya, Cambodia and a dozen other low-income countries, the All-Terrain Knee is sold at cost – the price of production – to ensure its affordability. Alternatively, people in developed countries are paying a higher price for a premium version of these knee joints. This “Tier-pricing system” allows the company to serve both low-income markets while sustainably providing a reliable product for clients in Canada and United States.
“Instead of costing $5,000, we want to bring that down to 1/10 of the market price,” says Jan, “Right now we are working with non-government organizations to ensure that people in developing countries have access to this technology, but also being able to receive support if necessary.”
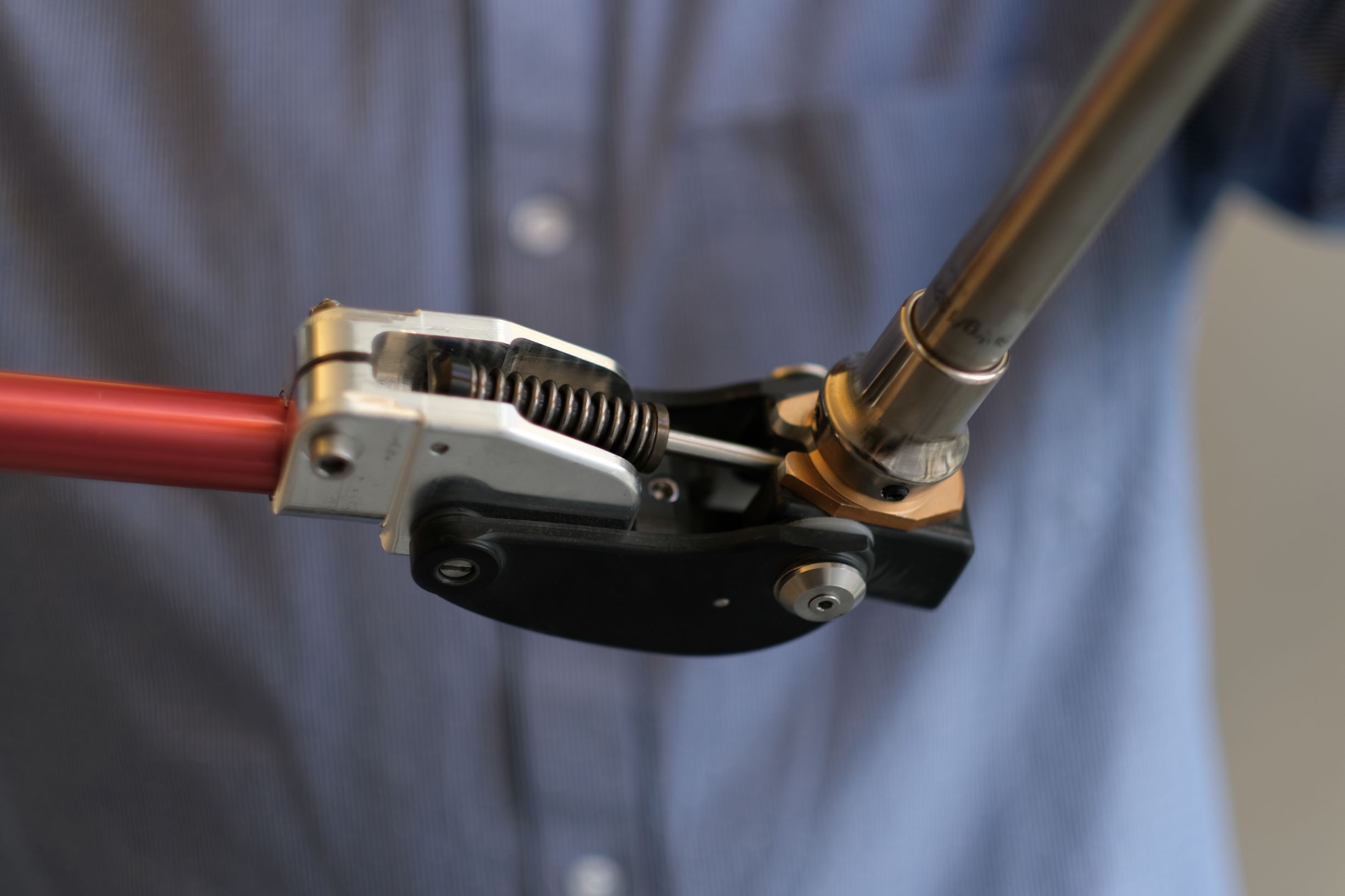
The knee joint utilizes a novel locking technology, to improve safety and minimize falls, while encouraging good walking patterns. Many patients who require these prosthetic devices are individuals who had suffered a previous injury or ailment that requires amputation, or congenital deficiencies at birth.
We are in the business of helping people, and if existing prosthetic devices are not reaching a wide audience, we are doing something terribly wrong.
The life-style requirement for these prosthetic devices also differ between countries. In Canada, a gap in the market would be to use prosthetic devices for recreational uses such as sports. Whereas in developing countries, the All-Terrain Knee is often the primary means by which a person is able to conduct their daily activities, such as working or going to school. In both contexts, the durability and functionality of the knee are essential to ensure that the user can conduct their necessary activities, in a safe and efficient manner.
The technology itself is completely operates without mechanical parts, meaning, there is no circuitry that interfaces with the mechanical movement of the knee and the biological parts of the leg. The lack of circuitry means these devices can be used in moisture dense and dirt rich environments without compromising its function. The knee joint locking mechanism is based on advanced biomechanics and works between two states. When pressure is applied on the device, the mechanical parts lock in place to ensure stability. While the patient is swinging the leg, the device engages the second state as the mechanical part releases to enable freedom of movement.

While one part of Jan’s work is in product development, his lab is focused on understanding how humans move while they are working. The principles from these studies can then drive the design considerations for mobility assistive devices such as prosthetic knees.
“We are focused on understanding the biomechanical principles of movement, during walking and other higher end mobility activities. Right now we are developing sensors that we can attach to the knee and measures data like how much pressure is applied, wear and tear, and other crucial biometric information about the device and the human body,” says Jan, “if we can understand how each person walks and their mobility requirements, we can design and personalize a device that’s useful to them.”
A major issue with prosthetic usage is that the amputee patients are not habituated in using the prosthetic devices. Whereas healthy individual would have symmetrical gait between the two legs, an amputee would spend considerably more time on the healthy leg over the other. The lack of gait symmetry could lead to other health problems such as back-injuries.
“An important aspect after lower-limb amputation is to inform and correct asymmetrical gait patterns of prosthetic users.” says Rafael Escamilla Nunez, a PhD student in the Andrysek Lab, “To address this problem, we developed a biofeedback device that measures various temporal gait parameters on each leg. Then, this information is processed by a microcontroller attached to the waist, which has embedded the control algorithms to activate the vibrating motors. For instance, if the person is spending asymmetrical time on one of the legs, our device vibrates and tells the person to correct their gait. It’s basically a rehabilitation device that helps people to walk properly.”

Sensors are attached to the shoe to measure various gait parameters. 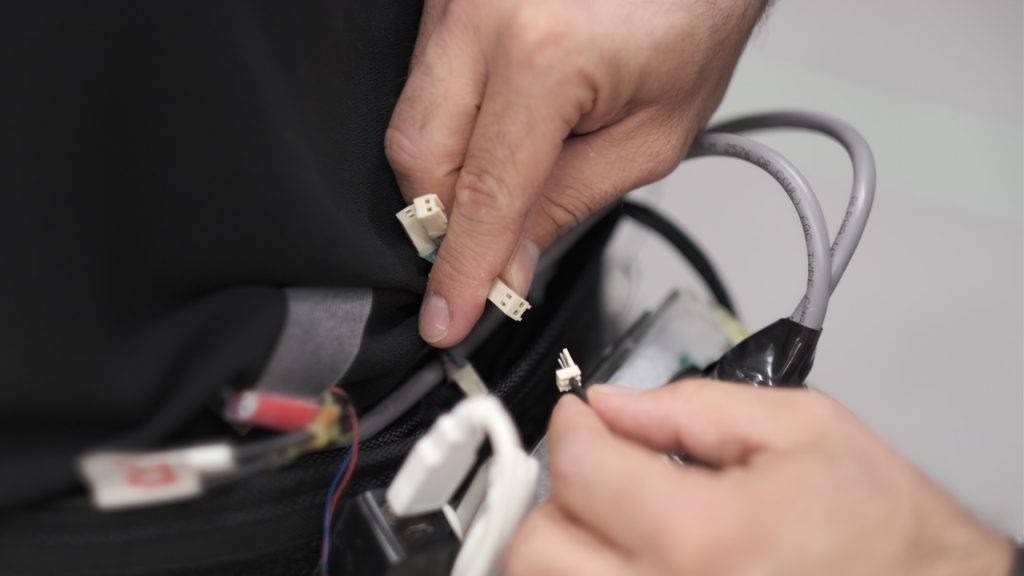
Microcontroller device that sends biofeedback signals to the leg.
Another issue is that some patients are also not confident with their usage of prosthetic devices.
“One of the patients we worked with initially had very little confidence in walking,” says Alexandria Michelini, a Masters student in the Andrysek Lab, “After a couple of rehabilitation sessions, she mentioned that she felt more confident and even started walking around the house a lot more. It feels great that our devices are making a difference in people’s lives.”■


