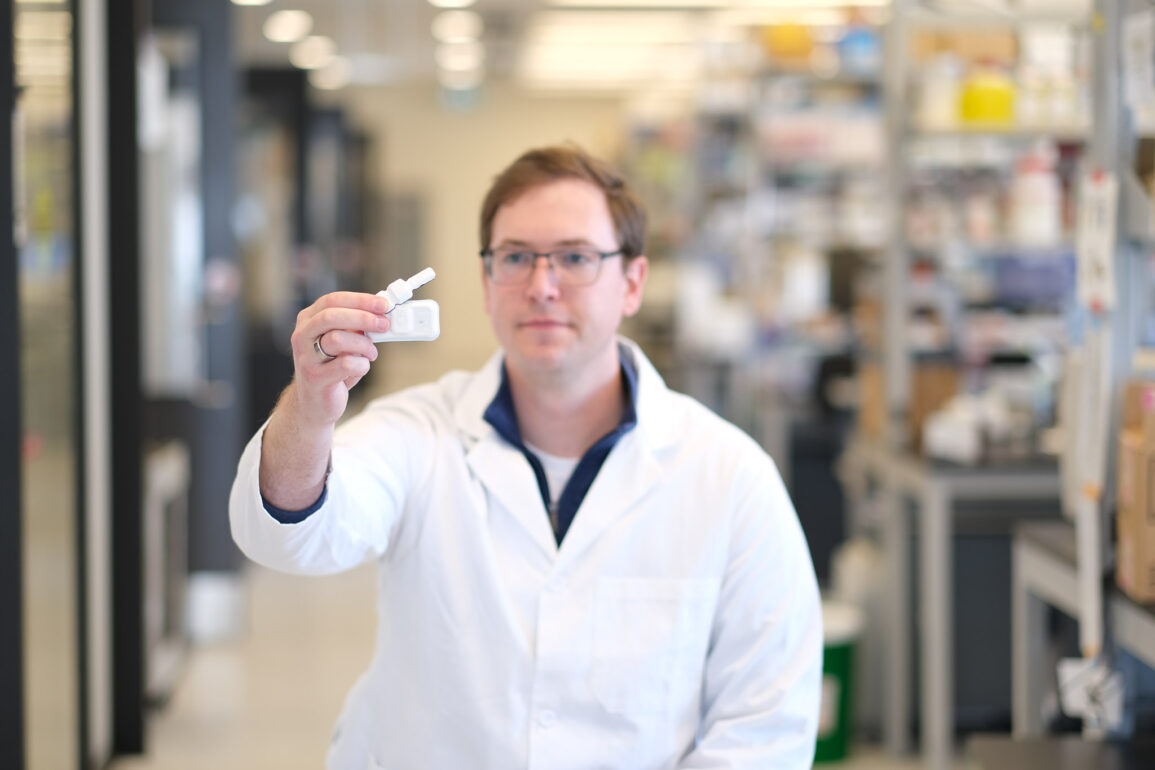
A team of researchers led by Professor Daniel Franklin (BME) from the University of Toronto Faculty of Applied Science and Engineering, Dr. Andreas Tzavelis, and Professor John Rogers at Northwestern University has unveiled a cutting-edge wearable medical device designed to revolutionize cardiovascular monitoring. This innovative device integrates multiple sensory modalities to provide a comprehensive assessment of hemodynamic status, surpassing conventional blood pressure monitoring. The findings were published in Nature Biomedical Engineering.
The device’s core innovation lies in its ability to measure not only blood pressure, but also correlates for cardiac output and vascular resistance, key indicators of the body’s regulatory processes for maintaining blood pressure. This addresses a critical gap in current monitoring methods, where underlying cardiovascular issues may go unnoticed despite normal blood pressure readings.
“Your body goes through great lengths to regulate and maintain blood pressure. If the ability of your heart to pump blood declines, say due to progression of disease, your body may compensate by constricting blood vessels to maintain blood pressure.” Said Professor Tzavelis.
The wearable system also enables remote monitoring, allowing patients to record data in their natural environments. This continuous stream of data provides a holistic view of an individual’s cardiovascular health, allowing for early detection and intervention from health care providers.
“This device offers a more comprehensive approach to quantifying an individual’s risk for heart failure and disease. Instead of periodic clinic visits, patients can now record data daily, providing invaluable insights into how their hemodynamic vital signs evolve over time,” said Professor Franklin.
The system consists of two devices—a chest patch and a peripheral device—that work in tandem. The chest patch, measuring approximately 44 centimeters by 70 centimeters, is attached using medical-grade adhesive. The peripheral device can be worn on the wrist or finger, allowing for versatile and personalized monitoring.
The technology behind these devices advances on that found within some commercial smart watches for non-invasive blood pressure measurements. Pulse arrival time, a well-established metric for estimating blood pressure, is used in conjunction with miniature spectrometers in the peripheral device. This enables the measurement of pulse wave dynamics as they propagate through the large arteries and the skin simultaneously, offering a deeper understanding of blood pressure and its regulation.
The devices are constructed using flexible printed circuit boards, encapsulated in medical-grade silicone. Their flexible design allows for various form factors, making them adaptable to different wearables, including wristbands, rings, and compact patches.
Moreover, these devices are hermetically sealed, ensuring water resistance and enabling them to be sterilized for medical use. They are wirelessly charged, eliminating the need for cumbersome connectors, or charging ports.
Professor Franklin acknowledges the collaborative effort that made this breakthrough possible. “It’s been a large team effort, with each member contributing their expertise in various aspects of the project.”
The project received support from the Ted Rogers Centre for Heart Research and was funded in part by TRANSFORM HF, a program aimed at advancing heart failure research.
With this wearable medical device, Professor Franklin and his team are poised to redefine cardiovascular monitoring, providing a new level of insight and precision in managing heart health.